
There are numerous innovative treatments for pinched nerves in the back. Pinched nerves develop when excess pressure is placed on a nerve from surrounding structures, including herniated disc, cartilage or boney spurs. The cause of your pinched nerve often influences what treatment or surgery will be most effective for you.
A pinched nerve can develop in the neck and upper spine, middle back and lower back, sometimes causing radiating pain down the legs. While a pinched nerve can form in other parts of the body, the spine is one of the most common areas to develop a pinched nerve.
Fortunately, non-surgical treatments are available to alleviate pain without the need for extensive surgery or downtime. For more severe symptoms, a spinal physician may recommend a surgical procedure if symptoms don’t improve with non-surgical treatment. Learn how to heal a spinal pinched nerve and promote your health.
Pinched nerves are a common condition, affecting approximately 85 out of every 100,000 adults in the United States each year. While anyone can develop a pinched nerve, they are most common in people 50 or older because of spinal degeneration and arthritis.
Some of the most effective spinal pinched nerve treatments are lifestyle-oriented changes. Pinched nerves originate from various conditions, meaning general lifestyle changes can help you find relief from discomfort even if the pain has multiple causes.
In some cases, you may need surgery or specific medical treatments for a pinched nerve caused by a specific condition. While you and your physician work to understand the cause of your back pain, general lifestyle changes can significantly improve immediate symptoms. Some of the most effective treatments for spinal pinched nerves in the back include:
A simple treatment for a pinched nerve is assessing and correcting poor posture. Sitting, lying or twisting in certain positions may aggravate or worsen back pain. A healthy posture can alleviate some strain and tension on the back, reducing the severity or frequency of pain.
For example, someone looking for treatment for a pinched nerve in the neck may need to correct their overall posture. Those with nerve pain in the neck may notice lying on their back can place strain on a painful neck. Some people find relief from this pain by adjusting their posture or entering the fetal position, alleviating overall pressure on their neck.
While adjusting your posture can be very helpful in minimizing pain, discomfort and other negative symptoms, each person is unique. In most cases, patients may need to experiment gently and note what positions feel better or worse. If any position causes even slight discomfort, you should avoid this position to minimize strain on the pinched nerve.
Oral medication, both over-the-counter and prescription, can improve pain and discomfort. Numerous types of pain medication are available, and some of the most commonly recommended medications for back pain are over-the-counter pain relievers, including non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen.
NSAIDs include naproxen and ibuprofen, which are both over-the-counter drugs that can correct inflammation, fever and pain. Acetaminophen can alleviate pain from a pinched nerve by blocking the transmission of pain signals to the brain.
A physician may also recommend muscle relaxants to help tense, sore muscles relax and release tension. Unlike NSAIDs and acetaminophen, muscle relaxants are prescription medications. Physicians may suggest opioids for severe or chronic back pain. While opioids effectively relieve pain, physicians don’t recommend opioid use in the long term.
Heat and cold therapy are ideal treatments to improve back pain from a pinched nerve. In general, if your pain is recent, you may want to apply an ice pack or cold compress for pain relief. Ice therapy can prevent excess inflammation and swelling. You can also gently massage a painful area of your back with an ice cube or cold compress.
When initial pain begins decreasing, you can switch to heat therapy or warm compresses. Heat helps relax sore, tight and irritated muscles, especially those around a pinched nerve. Another benefit of heat therapy is increasing circulation, promoting the healing process.
While warm compresses are helpful, electric heating pads can provide constant warmth to ensure comfort and pain reduction. You should place a towel between your heat source and your body to protect your skin from coming into contact with intense heat. You can apply heat to a pinched nerve for about 10 to 15 minutes.
A back or neck brace can support the spinal cord, minimizing excess movement of the back or neck. In most cases, a back or neck brace is meant for short-term use while you recover from an injury or flare-up of pain. When you have a pinched nerve, your spinal column may need additional support.
Braces help keep your spine in proper alignment and promote ideal posture to relieve the pressure and tension poor posture places on sore spinal nerves, joints and muscles to minimize pain. Another benefit of a back or neck support is that it allows you to perform daily tasks with minimal strain on the back or neck.
A back or neck brace is especially helpful at alleviating pain and tension when performing certain activities, such as lifting and bending. Although braces can help relieve pain, you should always use proper lifting techniques to minimize the risk of an injury.
Physical therapy and guided exercises are excellent ways to alleviate back pain from a pinched nerve and minimize other uncomfortable symptoms. When you go to a physical therapist, they will assess your unique symptoms and create a customized physical therapy plan for your needs.
There are passive and active physical therapy treatments depending on the severity of your symptoms and range of mobility. Physical therapy helps improve spinal health by increasing flexibility and strength. When the muscles of your spine are stronger and more flexible, they can better support sore areas, such as where a pinched nerve is located.
Physical therapy is an effective treatment for spinal pinched nerves and related pain because it helps improve spinal health at the source of a pinched nerve rather than simply masking the pain. Stronger spinal muscles can minimize the risk of injury, improving coordination, posture and balance.
An epidural steroid injection (ESI) is an effective treatment for various causes of lower back pain, including a pinched nerve. In many cases, epidural steroid injections are used in combination with other non-surgical pinched nerve treatments. During an epidural steroid injection, a specialist will inject a local anesthetic and steroidal medication into the epidural space surrounding the nerve roots and spinal cord.
Epidural steroid injections can enhance function and mobility in the lower back by reducing inflammation and irritation around the nerve roots. An epidural steroid injection can minimize pain, allowing you to participate in a rehabilitation and physical therapy program safely.
While epidural steroid injections are highly effective at minimizing pain, physicians may be more likely to suggest other non-surgical treatments first. If you don’t experience improvement of symptoms from other non-surgical treatments, a physician may recommend epidural steroid injections.
If you don’t experience pain relief from non-surgical pinched nerve treatments, your physician may recommend spine surgery. Spinal surgery can treat back pain at its source. Persistent back pain affects 16 million adults in the United States and is the sixth most costly medical condition. Fortunately, there are numerous types of spinal surgery available, including:
Endoscopic discectomy is a common surgery for spinal pinched nerves in the lower back. An endoscopic discectomy can also address pinched nerves in the middle back. During an endoscopic microdiscectomy, a spinal surgeon can directly visualize the spinal nerves and discs.
A spinal surgeon can decompress the nerve roots that are compressed and damaged by spinal discs. While an endoscopic discectomy is an effective surgery to alleviate pinched nerve pain, a physician will often initially suggest a more conservative treatment.
If you don’t experience relief from non-surgical treatments, a physician may recommend an endoscopic discectomy. Endoscopic discectomy is an ultra/least invasive surgery, meaning there is less soft tissue and muscle damage. With less damage, patients generally experience a shorter recovery period.
In most cases, patients experience immediate relief from pain and discomfort of a pinched nerve. Fortunately, there is minimal discomfort or pain following endoscopic discectomy. There are also fewer risks and complications than minimally invasive surgeries, including open spine surgery.
During an endoscopic discectomy, a surgeon uses a smaller incision (¼ inch versus 1-2 inches in minimally invasive), meaning there is very minimal scarring. Endoscopic discectomy has a high success rate and is a reliable treatment for pinched nerve pain. Additionally, there is little to no blood loss because the incision is smaller.
Endoscopic foraminoplasty is the least invasive spinal surgeries available to treat a pinched nerve in the neck or back that decompresses and frees a nerve. Foraminoplasty is a surgical procedure that enlarges the surrounding area of the spinal bone located near a pinched nerve.
This spinal surgery can alleviate compression and pressure on the nerves. During foraminoplasty, a spinal surgeon will make an incision in the neck or back, depending on the location of your pinched nerves. Next, the spinal surgeon can widen the intervertebral foramen to remove any blockages or causes of compression surrounding a nerve.
Foraminoplasty is an effective spinal treatment that is a less invasive alternative to spinal fusion surgery. Foraminoplasty can promote spine and muscle preservation. The incision used in foraminoplasty is one of the smallest incisions available during spinal surgery.
A smaller incision means less blood loss and a shorter recovery time with minimum scarring. In many cases, a spinal surgeon uses local anesthesia or mild sedation instead of general anesthesia, which often carries more risks. A foraminoplasty is an outpatient surgery, meaning patients can go home the same day of their surgery.
While each patient is different, the general healing time following a foraminoplasty is two to three weeks. You should follow all of your surgeon’s instructions to minimize the risk of complications and promote a smooth healing and recovery process.
A laminectomy is a minimally invasive surgical procedure that removes a small portion of the lamina bone, the bony sheath surrounding the spinal canal. Removing a part of the lamina allows a spinal surgeon to alleviate pressure and strain on the pinched nerve.
Along with the lamina, a spinal surgeon may remove a small portion of the tissue and other surrounding structures from the spine that are impinging on or worsening spinal health. With advancements in technology, a surgeon can perform a laminectomy with minimally invasive techniques to be more effective and mitigate risks of complications.
Generally, spinal specialists recommend a laminectomy for pinched nerves developing from a herniated disc, spinal stenosis or other spinal condition. Some cases of spondylolisthesis may also benefit from a laminectomy. During a laminectomy, a spinal surgeon will remove the bony spinous process.
Next, the surgeon will remove the bony lamina and thickened tissues connecting the laminae of the vertebra below. A laminectomy is a highly effective surgery to improve pain relief caused by pinched nerves.
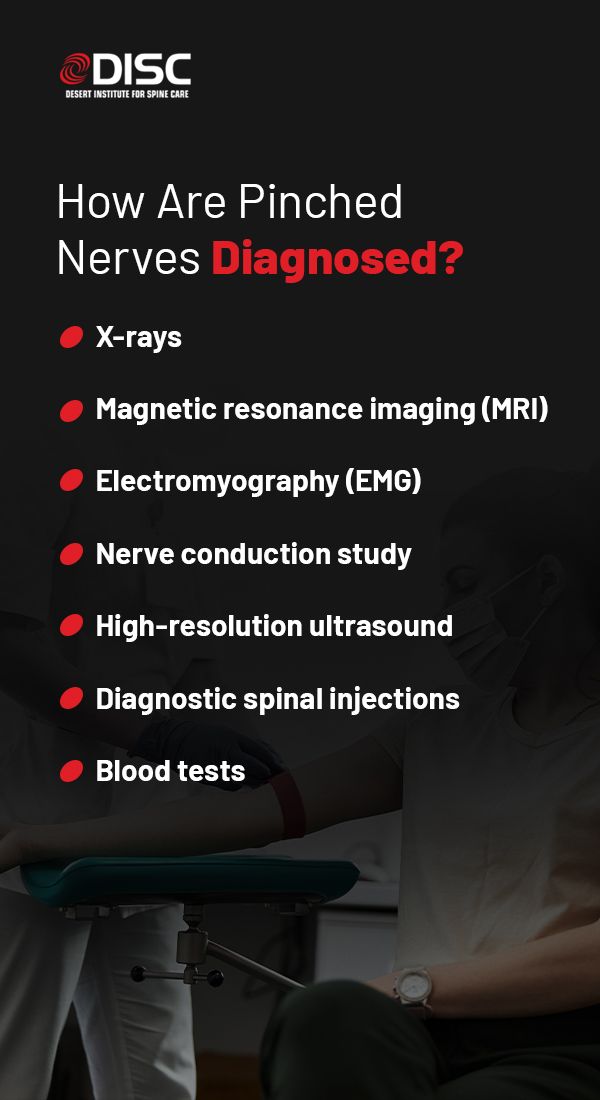
A spinal specialist will ask you about any spinal pain or symptoms you may be experiencing and often perform a physical assessment of your spine. If your physician thinks you are displaying pinched nerve symptoms, they will recommend further testing to diagnose your condition accurately. Some of the most important diagnostic tools for a pinched nerve include:
X-rays are one diagnostic tool a spinal specialist may recommend to diagnose a pinched nerve. An X-ray provides physicians with imaging of the spinal bones, allowing them to determine if there is a narrowing of the spinal column or other bone-related complications resulting in or worsening a pinched nerve.
An MRI is especially useful if your spinal physician suspects you may be experiencing pain from nerve root compression. MRIs use radio waves and a strong magnetic field to create detailed images of the spinal column and body. Where X-rays show the spinal bones, MRI images show a surgeon the soft tissues surrounding the bones, like nerves, spinal disc and ligaments.
An EMG involves inserting a needle electrode through the skin into the body’s muscles to evaluate the electrical activity present in the muscles when they are at rest or contracting. A physician can use the results of an EMG to determine if there is any damage to the spinal nerves and muscles.
A nerve conduction study measures the body’s electrical nerve impulses and the health of the nerves and muscles through electrodes placed on the skin. Your physician will pass a small current through the nerve to measure electrical impulses related to your nerve signals. Nerve conduction studies can help a physician detect potential nerve damage.
A high-resolution ultrasound uses sound waves to create images of the body’s internal structures. Ultrasound technology is especially effective in diagnosing nerve compression syndromes, including pinched nerves.
A surgeon can strategically place diagnostic injections at key spinal levels to confirm or relieve a patient’s source of pain. Once the source of pain is confirmed, a physician can customize a treatment to fit your unique symptoms and needs.
In some cases, your physician may recommend a blood test to assess thyroid levels or fasting blood glucose readings.
At the Desert Institute for Spine Care, we are world leaders in endoscopic spine surgery and helping patients live a pain-free life. Our surgeons are proud to offer the latest and most effective surgeries and use minimally invasive techniques to minimize post-operative healing and recovery times.
Our spinal treatments include artificial disc replacement, endoscopic spinal surgery, personalized pain mapping and more. We are experienced professionals able to detect and diagnose various spinal conditions, including radiculitis, failed back surgery syndrome and scoliosis.
Contact our spinal specialists online to learn more about our treatments and surgeries.