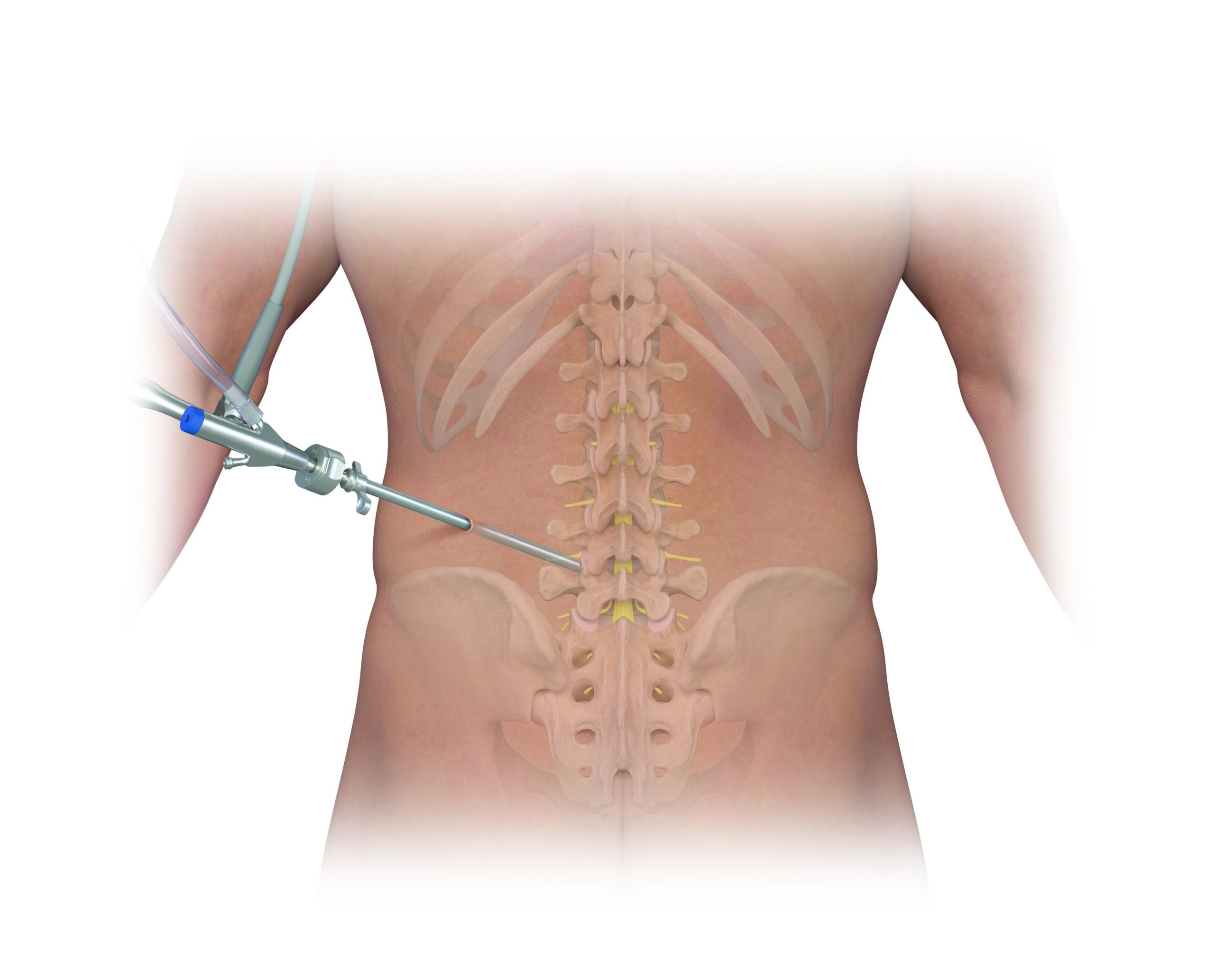
- What it is: Artificial disc replacement is a surgical technique in which a degenerated or damaged spinal disc is removed. An artificial disc made from metal or plastic is then used to replace the compromised spinal disc. Unlike fusion procedures, ADR maintains natural spinal motion, allowing for continued flexibility and function. Patients undergoing ADR often experience reduced pain, improved mobility, and a quicker return to daily activities. Artificial disc replacement can be performed in the neck or lower back.
- How it works: The goal of ADR is to preserve the natural motion of the spine. Unlike spinal fusion, which fuses vertebrae together, ADR allows the spine to continue moving in the same way it did before the injury or degeneration, helping to maintain flexibility and reduce pain.
- When it’s used: ADR is typically used when patients have DDD or herniated discs, particularly in the lumbar (lower back) or cervical (neck) spine regions.
Common Questions
Explore some of the common questions around ADR procedures:
What Is the Cost of Lumbar/Cervical ADR, and Is It Worth It?
The cost of a lumbar or cervical ADR depends on:
- The type of disc used.
- The surgeon’s fees.
- Hospital or surgical center charges.
- Whether it’s a cervical or lumber ADR.
Consider the following to determine if ADR is worth it for you:
- Degree of pain
- The pain’s impact on quality of life
- Your individual goals and expectations
- If conservative treatments have failed
What Are the Pros and Cons of ADR?
Some pros include:
- Pain relief.
- Improved function.
- Potential lowered risk of Adjacent Segment Disease (ASD).
Cons to keep in mind:
- Surgical risks, like anesthesia complications and infection.
- Potential disc dislocation.
- Not all patients are candidates.
Who Is a Candidate?
Any adult who has been experiencing significant lower back pain for a minimum of six months and where conservative treatments don’t bring full relief is a candidate.
What Is the Success Rate?
When patients are appropriately selected and pass candidacy, ADR has a relatively good success rate, averaging over 85%.
How Long Does an ADR Last?
ADR devices should last a few years, according to most manufacturers. ADR procedures that have been done five to 10 years ago still show promising results.
Does Insurance Cover ADR?
Yes, most major insurance providers cover ADR, but the coverage is based on the cost of the procedure, risks, and outcome benefits.
How Long Does It Take to Recover From ADR?
Different recovery times apply to lumbar and cervical ADR:
- Cervical ADR: Recovery time is usually short, and you can engage in light exercise within a week after the procedure.
- Lumbar ADR: With lumbar ADR, the abdomen has to heal, and you can start with low-impact exercises by the second month after having the surgery.