What to Expect from Cervical Artificial Disc Replacement Surgery
Our expert surgeons perform cervical artificial disc replacements as a minimally invasive procedure. Here is a quick look at the whole surgical process from start to finish.
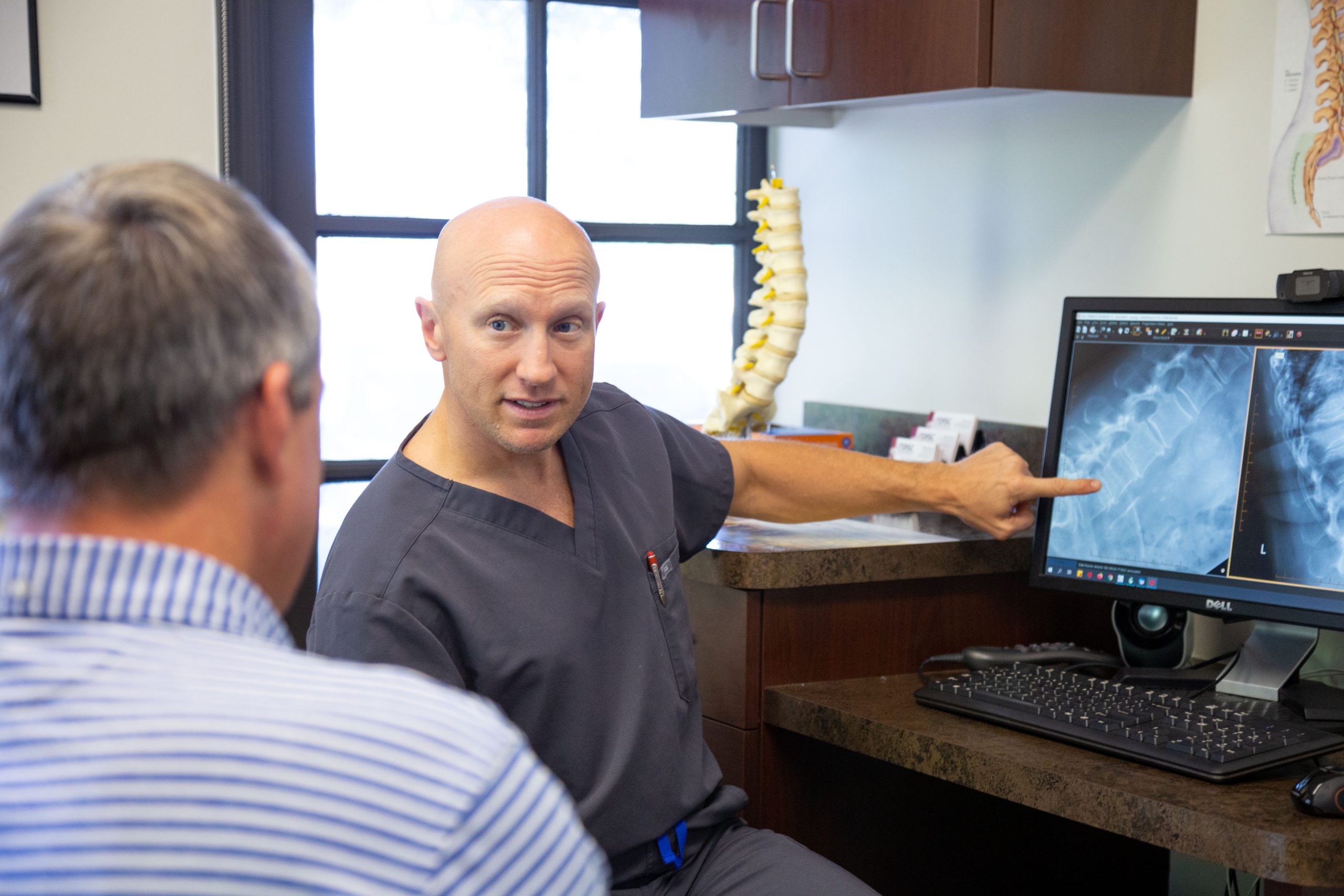
What Happens at a Pre-Operative Surgeon Visit?
During a pre-operative visit, a surgical patient goes through several important steps to ensure they are ready for the upcoming procedure. The healthcare provider will begin with a medical history review, examining any previous surgeries, chronic conditions, allergies, and current medications. A physical examination will follow to assess the patient’s overall health and identify any potential issues that might affect the surgery. Various preoperative tests, such as blood work, electrocardiograms (EKGs), chest X-rays, or other diagnostic tests, may be ordered to evaluate the patient’s health and readiness for surgery. Additionally, the patient will meet with an anesthesiologist to discuss anesthesia options, review any history of anesthesia reactions, and plan for the safest anesthesia approach.
The patient will receive instructions on which medications to continue or discontinue before surgery, often including the cessation of blood thinners or NSAIDs that could increase bleeding risk. Patients will be advised to avoid smoking and drinking alcohol before the surgery, as these habits can affect healing. They will also be instructed to fast, typically from midnight before the day of surgery, to ensure an empty stomach during the procedure. The patient will be provided with information about the surgery, including risks, benefits, and what to expect during recovery, and will sign a consent form to acknowledge understanding and agreement to proceed. Finally, logistical planning will be discussed, including arrangements for transportation to and from the hospital and plans for post-operative care, ensuring the patient has the necessary support at home. By the end of the pre-operative visit, the patient should have a clear understanding of the surgical process, be prepared for the day of surgery, and know what steps to take to optimize their recovery.
What Happens the Day of Surgery Before Cervical Disc Replacement?
In the pre-operative area at the hospital, several important steps are taken to prepare the patient for surgery. Upon arrival, the patient will check in, receive a hospital bracelet, and have their identity and surgical details verified. Nurses will then take the patient’s vital signs and conduct an initial assessment, asking about recent health status and any last-minute concerns. An IV line will be inserted to administer fluids, medications, and anesthesia. The surgeon may mark the surgical site to prevent wrong-site surgery, and the patient may receive preoperative medications such as sedatives and antibiotics. The anesthesiologist will review the patient’s medical history, discuss the anesthesia plan, and answer any remaining questions.
The surgical team will conduct a final verification process, often referred to as a “time-out,” to confirm the patient’s identity, the correct surgical procedure, and the correct site. The patient will also reconfirm their consent for the surgery. They will change into a hospital gown and remove any personal items. A final preoperative briefing will be given, including post-operative care instructions and what to expect immediately after the surgery. Finally, the patient will be transported to the operating room on a stretcher, where the surgical team will begin the procedure. Throughout this process, the medical team ensures that all necessary precautions are taken to maximize the safety and success of the surgery.